What is DBT and does it work?
Dialectical Behaviour Therapy (DBT) is a therapeutic method deriving from Cognitive Behavioural Therapy (CBT), and includes mindfulness and acceptance-based strategies in the client's treatment. The “D” in DBT refers to “Dialectical” which is a concept stemming from Zen tradition involving the synthesis of opposites, which allows us to see our experience in more than just one way.
One of the primary goals of treatment in DBT is to support clients in the development of four categories of skills. These skills help clients to manage distress with greater ease, increase pleasant emotions and reduce unpleasant ones and improve interactions with others.
DBT was first developed for clients with Borderline Personality Disorder, a population characterized by emotion dysregulation. DBT is now widely used to treat other mental health concerns, including anxiety and mood disorders. The comprehensive model of DBT was designed to be completed in one year and include individual therapy, skills group, phone coaching, and consultation team.
This article details the origins of DBT, the core reasons for success in therapeutic application, an in-depth look at the four major pillars of DBT skills, and an overview of the ways in which you can understand if DBT is right for you.
Origins and evolution of DBT
DBT was first designed in the 1970s for clients with Borderline Personality Disorder by a psychologist named Dr. Marsha Linehan who previously had the diagnosis herself.
Taking a dialectical stance allows us to see that two seemingly opposing and contradictory perspectives can both be true and be valuable to the situation at hand. For example, you can accept an emotion AND want to change the emotion; you can understand why someone behaved a certain way AND disagree with their behaviour.
One of the most important dialectics in DBT is the balance in acceptance and change. This is both a dialectic that is practiced by the therapist and one that is encouraged in their clients, allowing clients to make leaps forward in their treatment.
The “B” in DBT refers to the behavioural framework that we work from in therapy. In therapy we assess for behaviours, including their antecedents and consequences, which allows us to target and change specific behaviours (thoughts, emotions and actions) that interfere with one’s life goals. This allows us to find areas of patients’ lives where we can remove ineffective behaviours and replace them with skillful responses.
How does it work?
The comprehensive model of DBT is traditionally completed over one year and includes individual therapy, skills group, phone coaching and consultation team. While most research has explored the comprehensive DBT model with people experiencing Borderline Personality Disorder, more recently DBT has been increasingly used and proven effective for a wide range of mental health conditions.
DBT skills training groups are often offered either independently or adjunctive to one-on-one therapy, especially when comprehensive DBT is not available or unfeasible. A growing amount of research (1) is also suggesting that DBT skills groups or DBT skills taught in individual therapy settings can be effective in helping people cope effectively with their emotions by improving the way they experience, regulate and express their emotions.
Many of the difficulties that clients face are a result of skills deficits. What this means is that people may not have the coping skills or not know how or when to effectively implement them when experiencing volatile emotions. Clients often struggle to skillfully navigate challenging situations and may rely on ineffective coping strategies that can function as a way to avoid distress in the short-term (i.e. avoidance, aggression, substance use, self-injury) that create long-term consequences.
Too much of a focus on change can result in clients feeling invalidated or misunderstood, leading to less progress in therapy. By balancing behavioural change with acceptance, clients and therapists can work collaboratively to make improvements in therapy. Thus, a combination of behaviourism and dialectics can result in effective progress in emotionally sensitive clients.
DBT skills explained
In a nutshell, one of the goals of treatment in DBT is to support the client in developing skills for mindfulness, emotion regulation, crisis management and interpersonal relationships. Research has found that DBT skills can fully or partially explain improvements during DBT in problems such as suicidal behavior, non-suicidal self-injury, depression, anger control, emotion dysregulation, and anxiety (2)(3).
The following section will outline the four main categories of skills development in standard DBT.
Mindfulness
Mindfulness skills taught in DBT are ones that increase present moment focus, reduce judgmental thinking and improve intentionality when making decisions.
An example of a mindfulness approach that a client would use in and after DBT could be the learned ability to pause in the midst of an emotional episode and achieve greater awareness of the emotions and subsequent urges to manage the experience more skillfully as a healthy coping skill.
Distress tolerance
Distress tolerance skills are those that help to reduce the intensity of distressing situations and accept the reality of the moment, so that clients can get through overwhelming situations by tolerating the pain rather than engaging in ineffective behaviours (i.e. self-harm) to alleviate the pain.
Some examples of distress tolerance strategies include:
- Making an effort to improve the quality of the present moment
- Self-soothing by using the five senses
- Distraction from the distressor
- Using a pros and cons list to defer a problematic response to the stressor
Emotion regulation
Emotion regulation skills increase one’s capacity to identify and accept emotions, reduce unpleasant emotions, and increase the frequency of pleasant emotions. In practice, emotion regulation helps clients to identify, name, and change their emotions.
Interpersonal effectiveness
Interpersonal effectiveness in DBT is the learning of skills to improve interactions with others and enhance one’s ability to navigate difficult interpersonal situations.
This kind of skills training helps the client to become more assertive and effective in their relationships. An example of this assertiveness could be the expression of one’s needs and the ability to say no to others without damaging relationships.
The following graphic outlines these four pillars of DBT.
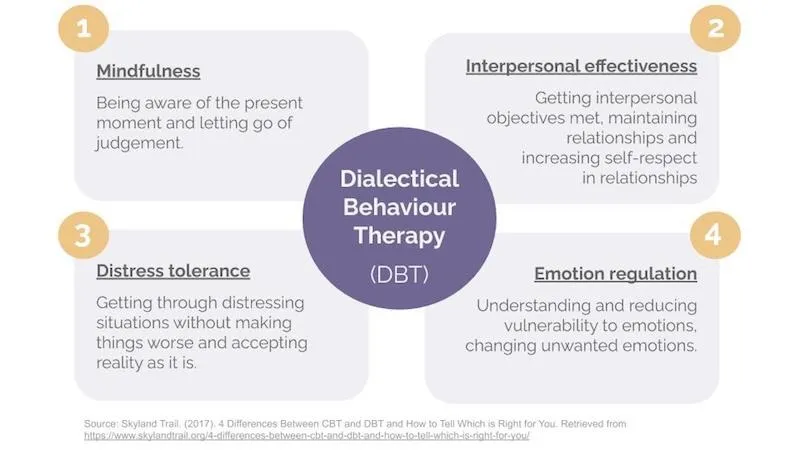
Image of the 4 core skills of Dialectical Behaviour therapy (DBT) - Mindfulness, Interpersonal effectiveness, Distress tolerance, Emotion regulation
Another final defining attribute of DBT centers around the therapist's approach, rather than the client’s mental health concerns and subsequent skills training.
In traditional DBT therapy, the therapist will focus on holding clients accountable, and will often be bit more direct than in traditional therapy.
When is DBT right for you?
DBT may be right for you if:
- You seem to be more emotionally sensitive than other people.
- Your emotions are experienced as very intense and you act impulsively without considering the consequences of your actions.
- Your emotions seem to take over causing you to act out in unhelpful ways, while other times you bottle them up inside to appear on the outside as if everything is fine.
- You avoid the experience of unpleasant emotions and as such often feel numb or empty.
- Emotions get in the way of you achieving your goals, such as holding a job, maintaining friendships or pursuing your interests.
- You’ve had a history of relationships that have ended abruptly and you tend to have conflict in many of your relationships, whether with family, friends, your partner or other important people.
- You don’t trust others or that relationships will work, so you withdraw from others to avoid rejection, abandonment or being hurt by others, which leads to loneliness.
- You struggle to know your true identity because your values, behaviours and personality change between situations and groups of people.
- You struggle to use coping skills to solve your problems and end up making poor decisions in an attempt to relieve your emotional pain.
To learn more DBT and other available treatments, speak to your primary care physician or to your mental health health provider for advice specific to your personal health profile.
DBT is helping clients around the world to address common skills deficits by developing coping mechanisms and the ability to identify when those means should be implemented to address volatile emotions.
To learn more about community paid and funded DBT groups, head to the appendix below. If you’re looking for other available treatments, speak to your primary care physician or mental health provider for advice specific to your personal health profile. Or you can always speak to a Layla Care Coordinator for more information about seeking individual therapy with a therapist who is trained in DBT.
APPENDIX
DBT Community Resources and Groups
Publicly-funded Groups (FREE)
Trillium Health Partners (THP) Intensive Outpatient Program
- This skills based program runs a maximum of 12 weeks with a commitment of 3 hours per week. The program is designed to help clients develop tools and increase their support through the use of Dialectical Behavioural Therapy (DBT) and Cognitive Behavioural Therapy (CBT). A referral from a physician is required and should be directed to Centralized Intake at one-Link, who would conduct a screening call as eligibility requirements vary across programs. To see a psychiatrist, clients must meet specific eligibility standards, and the psychiatrist determines next steps in care. For certain diagnoses, documented medication trials are required before accessing some services. Please note that one-Link doesn’t directly place clients into THP or other specific programs. Its role is to help coordinate services and guide individuals to the most appropriate supports.905-338-4123
- A referral from a physician, nurse practitioner, or other authorized healthcare provider is required. Clients may be connected to the program through the Borderline Personality Disorder (BPD) Clinic, the Eating Disorders (ED) Clinic, or Psychiatry Consult Services.
- Ontario Shores Phone Number: 905-430-4055
- The CMHA Toronto Dialectical Behaviour Therapy (DBT) Program is a one-year intensive treatment designed for adults (18+) experiencing significant emotion regulation difficulties, including those diagnosed with Borderline Personality Disorder (BPD). A referral form is required to apply (physician referral or self referral). The program is currently full, but individuals may sign up to receive notification when referrals reopen. Upon completion, graduates may join the DBT Alumni Program for continued support.
- CMHA Phone Number: 416-789-7957
- CMHA Email: info@cmhato.org
Private Group (Paid)
- This service offers 12-week group programs, including a foundational Dialectical Behavioural Therapy (DBT) program and advanced program for those who have participated in DBT previously. Most programs are for adults 18+, but they also offer an adolescent program for ages 14-17. Sessions are $50-$70 per session and are available to clients in Ontario, British Columbia, Nova Scotia and Alberta. Participants can self-refer or be referred from a physician or community partner. DBT Virtual also offers free webinars which can be found here.
- DBT Virtual Phone Number: 289-203-3021
- DBT VirtualEmail: info@dbtvirtual.com
- CMBH offers Dialectical Behavior Therapy (DBT) Skills Training, Dialectical Behaviour Therapy (DBT) Graduate Skills and a Dialectical Behaviour Therapy (DBT) Family and Friends Support Group. Sessions are $140 per session and the program runs for 12 weeks with a 2 hour commitment per week. No referral is required to access services.
- CMBH Phone Number: 647-729-5551
- Broadview Psychology offers a DBT skills groups for different age groups (children, adolescents, young adults, and adults) and stages of support. These groups run weekly for 6–9 months, mostly in person, though some virtual options are available. In addition, there are DBT parent and family groups, providing training and support for parents, caregivers, partners, and family members across different age ranges. Costs range from $105-$140 per session. Intake is continuous, meaning clients do not have to wait for a cohort to start treatment. Clients are required to be simultaneously meeting with an individual therapist either through their clinic or externally.
- Broadview Psychology Phone Number: 647-348-5140
Free Self-Guided Resources
- Free DBT Skills Webinars led by trained DBT experts.
- Free Video Modules for Dialectical Behavioural Therapy
Sources:
- Jennifer Urbano Blackford and Rene Love. (2012). Dialectical Behavior Therapy Group Skills Training in a Community Mental Health Setting: A Pilot Study. National Library of Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191933/
- Andrada D Neacsiu, et. all. (2010). Dialectical behavior therapy skills use as a mediator and outcome of treatment for borderline personality disorder. National Library of Medicine. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20579633;
- Andrada D Neacsiu, et. all. (2014). Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: a pilot randomized controlled trial. National Library of Medicine. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24974307
- Seth R Axelrod, et. all. (2010). Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. National Library of Medicine. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21091162



